Spine
Neck and lower back pain are common occurrences in the general population. It is estimated that approximately 80% of the population will experience pain in the lower back and/or neck at some time in their life. Fortunately, most cases can be resolved without surgical treatment. Our specialists are dedicated to understanding the most advanced treatment methods for particular problems associated with the spine, neck, and back. When it comes to the treatment of spine disorders, Hinsdale Orthopaedics offers a comprehensive approach to spine assessment and treatment for our patients.
Our team of physicians is comprised of board certified, fellowship trained orthopaedic spinal surgeons focused exclusively on spine surgery and specializing in innovative surgical and nonsurgical interventions. Nationally and internationally respected authors and researchers in their field, the surgeons and practitioners at Hinsdale Orthopaedics serve as a referral center for some of the most complex cases of the human spine.
Anatomy
Cervical Spine Anatomy
Anatomy of the Spine
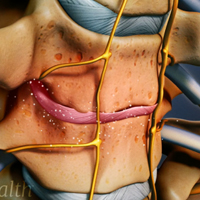
The spine, also called the backbone, plays a vital role in stability, smooth movement and protection of the delicate spinal cord. It is made up of bony segments called vertebrae with fibrous tissue called intervertebral disks between them. The vertebrae and disks form the spinal column from the neck to the pelvis, giving symmetry and support to the body.
Parts of a Vertebra
A single vertebra is made up of two parts, the front portion is called the body and the back portion is referred to as the vertebral or neural arch. The body is cylindrical in shape, strong and stable. Two strong pedicle bones join the vertebral arch to the body of the vertebrae.
The laminae of the vertebra can be described as a pair of flat-arched bones that form a component of the vertebral arch. The transverse processes spread out from the side of the pedicles like wings and help to anchor the surrounding muscle to the vertebral arch. The spinous process forms a steeple at the apex of the laminae and is the part of our spine that is felt directly under the skin.
Spinal Canal
The spinal canal is formed by the placement of single vertebral foramina one on top of the other to form a canal. The purpose of the canal is to create a bony casing from the head to the lower back, through which the spinal cord passes.
Cervical Spine Anatomy
The spine can be divided into 4 parts: cervical, thoracic, lumbar and sacral region. The cervical spine comprises of the first 7 vertebrae, which form the neck.
The cervical spine is highly mobile compared to the thoracic or lumbar spine. In contrast to other parts of the spine, the cervical spine has transverse foramina in each vertebra through which the vertebral arteries supply blood to the brain.
Based on the structural diversity in the cervical spine, it can be divided into two parts: the upper and lower cervical spine.
Upper Cervical Spine
The upper cervical spine comprises of the atlas (C1) and axis (C2), which are different from rest of the cervical vertebrae. The atlas vertebra articulates with the occiput superiorly at the atlanto-occipital joint and with the axis inferiorly at the atlantoaxial joint. Generally, the atlantoaxial joint is accountable for half of the cervical rotational movements; while the atlanto-occipital joint is responsible for half of the flexion and extension movements of the neck.
Atlas (C1)
In contrast to other vertebrae, the atlas is ring-shaped without a body. The odontoid process or dens of the axis represents the fused remnants of the body of the atlas. The transverse ligament firmly opposes the odontoid process to the posterior portion of the anterior arch of atlas and provides stability to the atlantoaxial joint.
The atlas comprises of a thick anterior arch, a thin posterior arch, two prominent lateral masses, and two transverse processes. The transverse process surrounds the transverse foramen, through which the vertebral artery passes. A zygapophyseal joint is present on the superior and inferior aspect of the lateral mass. The superior articular facets articulate with the occipital condyles and are kidney-shaped, concave, projecting upward and inward, while the inferior articular facets are comparatively flat, projecting downward and inward, and articulate with the superior facets of the axis.
Axis (C2)
The axis possesses a large vertebral body with the odontoid process or dens. It also has heavy pedicles, laminae and transverse processes that help in the attachment of muscles.
Lower Cervical Spine
The remaining five cervical vertebrae, C3-C7, form the lower cervical spine. They are similar to each other, but distinct from C1 and C2. Each of these cervical vertebrae has a body with a concave superior surface and convex inferior surface. The superior surfaces of the bodies have raised processes called uncinate processes that articulate with the inferior lateral portion of the vertebral body present above, called echancrure or anvil.
The C3-C6 vertebrae have bifid spinous processes, meaning they are split into two parts, while C7 has a non-bifid, rounded spinous process.
Intervertebral Disk
The intervertebral disks are flat and round, present between the lumbar vertebrae and act as shock absorbers when you walk or run. There is a soft, gelatinous material in the center (nucleus pulposus) that is encased in strong elastic tissue, forming a ring around it called annulus fibrosus.
Facet Joint
Facet joints are synovial joints that give the spine it’s flexibility by sliding on the articular processes of the vertebra below. Compared to other parts of the spine, the joint capsules are quite loose in the cervical region to facilitate smooth movement.
Conditions

Herniated Disc
Disc herniation is a condition where the central nucleus pushes through the outer edge of the disk, causing a bulge that compresses the spinal nerves

Low Back Pain
Low back pain is often a common symptom of many disease conditions and the back pain may range from simple or dull pain to sudden and sharp pain.

Sciatica
Sciatica is a painful condition caused by the irritation of the sciatic nerve. Sciatica can be acute (short term), lasting for a few weeks or chronic (long term), persisting for more than 3 months.

Scoliosis
Scoliosis is a condition characterized by the abnormal curvature of the spine that causes a deviation to one side. It causes a physical deformity, making the spine look like the letter “C” or “S” instead of the letter “I”

Spinal Stenosis
Spinal stenosis is a condition caused by the vertebral column constricting and exerting pressure on the spinal cord or neural foramen (a bony tunnel through which a nerve exits the spinal cord)

Spinal Tumors
A spine tumor is the abnormal growth of uncontrolled tissues or cells in and around the spinal cord. Tumors can either be cancerous (malignant) or non-cancerous (benign). Tumors that begin in the spine are called primary spinal tumors.

Spondylosis
Spondylosis is a condition where the bones that make up the spine (vertebrae) degenerate. Typically this degeneration forms bony projections (bone spurs) and reduces the height of the spongy discs between the vertebrae

Whiplash
Whiplash is a soft tissue injury to the neck, usually caused by a sudden forceful jerk commonly occurring because of an automobile accident, sports injuries or an accidental fall.

Vertebral Compression Fracture
Back pain is an indication of stress fractures known as vertebral compression fractures. Vertebral compression fractures occur when the normal vertebral body of the spine is squeezed or compressed.
Spine Bone Spurs
Spine bone spurs, also called osteophytes, are bony projections that develop in the spine’s facet joints where cartilage has worn out oralong the vertebral body’s endplates edges. It can grow at any level of the spinal column such as the low and mid back and in the neck.
Lumbar Spine Procedures
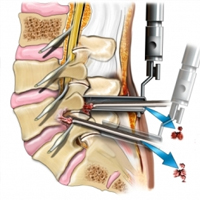
Endoscopic Spine surgery
Endoscopic discectomy,
is a minimally invasive surgical procedure used to remove herniated disc material that is causing pain in the lower back and legs (lumbar), mid back (thoracic), or neck and arms (cervical).
Endoscopic discectomy is the least invasive and most effective surgical technique for treating spinal disc herniation patients. With endoscopic spine surgery, surgeons do not need to remove bones and muscles in order to remove herniated discs. Surgeons can see the spine with a camera, smaller than a smart phone camera, through a small surgical port (tube). Large incisions are avoided. The procedure does not traumatize your spine like traditional spine surgeries do. The whole procedure for a disc herniation takes about 30 minutes. The patient goes home in 2-3 hours when the surgery is done.
Endoscopic Spine Decompression
An endoscopic micro-invasive decompression is the least invasive technique that allows direct visualization of the disc and the nerves. This procedure is used for decompressing nerve roots damaged by narrowing of the spinal canal and foramens caused by bulging disc, herniated discs, facet arthritis, bone spur, scoliosis, and spondylolisthesis
It is usually indicated in patients with neurological symptoms such as radiating pain down the legs, tingling, numbness, weakness, difficulty breathing, and in some cases bowel/bladder problems. Most of our patients have not found adequate relief with non-surgical modalities including but not limited to pain management injections or conservative treatments. This procedure can also help in relieving pain associated with spinal stenosis and low back arthritis.
What is an endoscopic decompression?
An endoscopic decompression is the least invasive surgery that allows the surgeon to decompress the spinal nerves in the spinal canal with less than 1 cam incision. The surgery is utilizing endoscope, real time EMG, real time radiographic images so the surgery is very safe and effective
Many patients who suffer from sciatica, referred pain down either legs, and/or low back pain may be a candidate for this procedure. This procedure can also help in relieving pain associated with spinal stenosis and low back arthritis.
Benefits associated with a Micro-invasive endoscopic decompression
- Least invasive technique – less trauma to muscles and soft tissue than with traditional open surgery
- Fast recovery time
- Minimal pain or discomfort following the surgery
- Immediate leg pain relief in most cases
- Fewer complications and risks than open spine surgery
- Small incision and minimal scar tissue
- High success rate and sustained success of the therapy
- No or minimal blood loss
- No hardware placement or loss of mobility
Endoscopic Facet joint rhizotomy
Endoscopic rhizotomy allows the spine surgeon to place a small cannula and an endoscope attached to an HD camera, inside the patient’s back and target visually the medial branch nerve. A radiofrequency probe is used through the endoscope to ablate the medial branch nerve. Because the endoscope allows us to see the medial branch nerves that cause low back pain, we can ablate and sever these nerves with certainty. Also, the endoscopic rhizotomy surgery provides much longer pain relief (up to 5 years) to patients than the traditional pain management RFA. This procedure has spared many patients of more invasive spine surgery such as a spinal fusion. patients have been very satisfied with the results and typically go back to work or an active lifestyle in a few weeks.
The advantage of the endoscopic rhizotomy is that it is often used when other surgeons have recommended no treatment at all or spinal fusion for the back. The procedure is less invasive and a great alternative for patients suffering from debilitating back pain and spasms.
- High success rates, 90% or above
- Utilizes an HD camera coupled to an endoscope which provides the physician a superior view to that of traditional surgical techniques
- No spinal fusion is necessary thus preserving the spinal column and the disc
- Less than i cm incision minimizes potential skin scarring
- No muscle or tissue tearing thus less scar tissue and preserve spinal mobility
- No significant blood loss
- Conscious sedation reduces the risk associated with general anesthesia
- Less post-operative pain and need for narcotic medicines
- Less recovery time needed
- Return to work sooner
What Conditions Does Endoscopic Facet Rhizotomy Treat?
- Facet joint syndrome
- Facet related arthritis
- Chronic low back pain
- Back spasms related to the facet joint
- Failed back surgery
Endoscopic sacroiliac joint rhizotomy
the sacroiliac joint can become inflamed and painful or injured for a number of different reasons.it is one of the most common causes of lower back pain, as in facet joint rhizotomy we utilize a small endoscope through a 5 mm incision and insert a radiofrequency probe through the scope in order to burn the sensory nerves supplying sensation to the Sacroiliac joints. The endoscope allows us to see the lateral branches (sensory nerves )and ablate them. patients have been very satisfied with the results and typically go back to work or an active lifestyle in a few weeks, this allows up to a five year pain free period. It also has superior results over thermal ablation by needles and SIJ steroid injections.
Endoscopic Coccygeal nerves rhizotomy
treatment of chronic coccyx related pain can often be difficult, especially when it comes to long term improvement. As with other pain management options, coccyx treatments can be temporary in that the goal is to alleviate the pain while the body attempts to heal itself. If the coccyx pain has become chronic, meaning that it has been persisting for over 6 months, it is less likely to get better and longer term treatment options have been less likely to improve the condition. Coccygectomy is no longer a good solution for coccygeal fractures, it carries major risks and complications as well.
The endoscopic radiofrequency ablation of the coccygeal nerves involves using an endoscope (small tube) through which the coccyx and its nerve supply can be directly visualized. Through the endoscope one can then insert small tools and then ablate/burn the nerves under direct visualization. The endoscope itself is similar to the small scope commonly used for arthroscopic surgery. Skin incision size is typically 0.5 cm long (less than ¼ inch) and requires only a small stitch under the skin to close.
Minimally Invasive Spinal fusion
Spinal fusion is a surgical procedure to join 2 or more bones of your spine together permanently. A minimally invasive spinal fusion uses a smaller cut (incision) than a traditional spinal fusion surgery.
Various medical conditions might cause your vertebrae to move against each other more than they should. This can stretch your surrounding nerves, ligaments, and muscles, causing pain. For example, if you have arthritis of your spine, your vertebrae might hurt when they move against each other. Spinal fusion may stop this pain by preventing 1 or more of your vertebrae from moving.
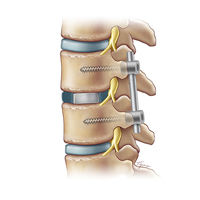
Transforaminal Lumbar Interbody Fusion TLIF
TLIF back surgery is done through the posterior (back) part of the spine.
- Surgical hardware is applied to the spine to help enhance the fusion rate. Pedicle screws and rods are attached to the back of the vertebra and an interbody fusion spacer is inserted into the disc space from one side of the spine.
- Bone graft is placed into the interbody space and alongside the back of the vertebra to be fused. Bone graftis obtained from the patient’s pelvis, although bone graft substitutes are also sometimes used.
- As the bone graft heals, it fuses the vertebra above and below and forms one long bone.
Extreme Lateral Interbody Fusion XLIF
The XLIF (eXtreme Lateral Interbody Fusion) is an approach to spinal fusion in which the surgeon accesses the intervertebral disc space and fuses the lumbar spine (low back) using a surgical approach from the side (lateral) rather than from the front (anterior) or the back (posterior).
XLIF Indications:
- Lumbar DDD
- Spondylolisthesis
- Scoliosis
- Lumbar Herniated Disc
- Lumbar Stenosis
The XLIF is one of a number of spinal fusion options that a surgeon may recommend to treat specific types of lumbar spinal disorders, such as lumbar degenerative disc disease, spondylolisthesis, scoliosis and deformity and some recurrent lumbar disc herniations and types of lumbar stenosis
Anterior Lumbar Interbody Fusion
The anterior lumbar interbody fusion (ALIF) is similar to the posterior lumbar interbody fusion (PLIF), except that in the ALIF, the disc space is fused by approaching the spine through the abdomen instead of through the lower back. In the ALIF approach, an incision is made on the left side or the lower part of the abdomen and the abdominal muscles are retracted to the side.
The ALIF approach is advantageous in that, unlike the PLIF and posterolateral gutter approaches, both the back muscles and nerves remain undisturbed.
Another advantage is that placing the bone graft in the front of the spine places it in compression, and bone in compression tends to fuse better.
Lastly, a much larger implant can be inserted through an anterior approach, and this provides for better initial stability of the fusion construct.
Spinal Disk Replacement
A lumbar disk replacement is a type of back or spine surgery. Your spine is made up of bones called vertebrae that are stacked on top of each other. Disks between the vertebrae work like cushions to allow the vertebrae to rotate and move without the bones rubbing against each other. The lumbar vertebrae and disks are at the bottom of your spine. Lumbar disk replacement involves replacing a worn or degenerated disk in the lower part of your spine with an artificial disk made of metal or a combination of metal and plastic.
Lumbar disk replacement is generally seen as an alternative to the more common spinal fusion surgery. Fusion permanently joins 2 vertebrae together, disc replacement preserves motion which is closer to natural disc. Lumbar disk replacement is a major surgery that requires general anesthesia and a hospital stay.
The main reason you would need a lumbar disk replacement is to treat low back pain. Still, not everyone with low back pain is a good candidate for a lumbar disk replacement surgery. Your doctor will need to do some tests to see if it’s the right procedure for you.
In general, lumbar disk replacement surgery might be recommended if:
- Your back pain mostly comes from only 1 or 2 disks in your lower spine
- You have no significant joint disease or compression on the nerves of your spine
- You are not excessively overweight
- You haven’t previously had spinal surgery
- You don’t have scoliosis or another spinal deformity